What is Audio-Only (Telephone) E/M?
CMS issued a waiver to allow the use of audio-only equipment to furnish services described by the codes for audio-only telephone E/M services, behavioral health counseling, and educational services.
Effective January 1, 2021, CMS established payment on an interim final basis for a new HCPCS G-code describing 11-20 minutes of medical discussion to determine the necessity of an in-person visit.
Components of Implementing Audio-Only E/M
Patient initiates & Consent
Acquire consent from the patient to be remotely monitor (verbal and written(Annually)
Enroll Requirements
Services can only be issued for established patients only
Monitoring and Billing
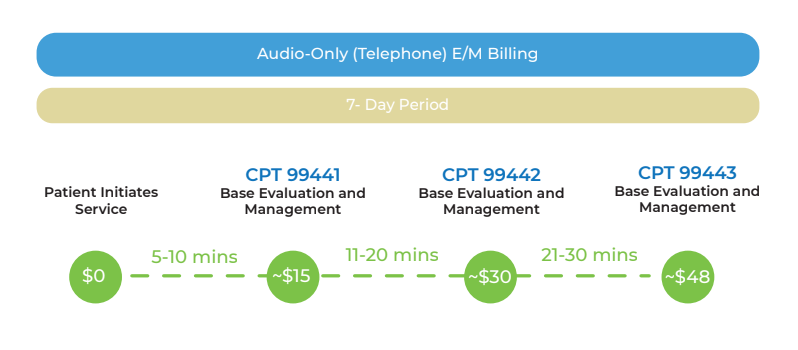
Services can be reported for billing once in a 7-Day period
The Workflow
Plan
Create an Audio-Only E/M work-flow, establish documentation, and billing procedure
Train
Train qualified clinical staff to help remotely monitor patients' vitals.
Consent
Acquire consent from the patient to be remotely monitored
Educate
Educate patients on how to measure oxygen and blood pressure health data using Connect+ to collect health data
Sync
Patient sync and health data remotely monitor by physician/clinical staff
Submit
Submit eligible patients for billing and get reimbursed for monthly monitoring
Audio-Only Evaluation & Management Path
Audio Only E/M CPT Billing Code Guide
CPT 99441
Audio-Only and Management Monitoring-
Telephone evaluation and management service by a physician or other qualified health care professional who may report evaluation and management services provided to an estab- lished patient, parent, or guardian not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment; 5-10 minutes of medical discussion)
CPT 99442
Audio-Only and Management Monitoring-
Telephone evaluation and management service by a physician or other qualified health care professional who may report evaluation and management services provided to an established patient, parent, or guardian not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment; 11-20 minutes of medical discussion
CPT 99443
Audio-Only and Management Monitoring-
Telephone evaluation and management service by a physician or other qualified health care professional who may report evalua- tion and management services provided to an established patient, parent, or guardian not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment; 21-30 minutes of medical discussion
Frequently Ask Questions
What is the difference between Telehealth services and telephone (audio only) calls?
Telehealth services are live, interactive audio and visual transmissions of
a physician-patient encounter from one site to another using telecommunications technology. They may include transmissions of real-time telecommunications or those transmitted by store-and-forward technology. Telephone calls (audio only), which are considered audio transmissions, per the
CPT's definition is non-face-to-face evaluation and management.
Do the reimbursement policy changes require me to bill differently?
Yes. Prior to Public Health Emergency temporary change, telehealth ser-
vices were required to be billed with POS 02 to identify them as telehealth services. We are suspending this requirement. In order to identify telehealth or telephone (audio only) services that were historically performed in the office or other in-person setting (E.g. POS 11, 19, and 22) modifier GT or 95 GQ for Medicaid)
must be used. Place of Service 02 will reimburse at traditional telehealth
rates. Audio-only CPT codes 98966-98968 and 99441-
99443 do not require telehealth modifiers to be reported.
If the patient was seen in the past seven days in the office or for a tele- health visit, and now calls for a phone-only consultation, can we still bill this as a virtual check-in (G2012) or a phone call (99441-99443, when they have that 7-day global period?)
For the virtual check-in code, G2012, I would say no. That was specifically tied to a “possible E&M” with the patient. So, if the patient was seen seven days prior for a related condition, it is an extension of that visit. As for the telephonic visits, 99441-99443 and 98966-98968, the CPT descriptor has similar rules regarding these codes, and CMS has not addressed them. In lieu of clear direction, I would follow CPT guidance. Reminder: phone calls are not telehealth, so do not add the modifier -95.